Anita Hedditch
The Oxford Breech Service
North of England Breech Conference, Sheffield
Day 2
This is the first of 3 hospitals presenting about starting a vaginal breech service. The other hospitals include The Jessop Wing in Sheffield and Sachsenhausen Hospital, Frankfurt, Germany.
Anita Hedditch is a midwife at Oxford University Hospital and has been in practice since 1992, allowing her to witness the changes brought about by the Term Breech Trial. She leads a group of midwives who provide 24/7 access to upright breech birth. She has also been involved with Oxford's ECV clinic since 2010. Established in 1999, the ECV clinic has a database of 2,500 ECV attempts. The Oxford Breech & ECV Clinics are also the home of the Greentop Guideline for Breech Presentation (headed by Lawrence Impey).
In the beginning, establishing a breech service at Oxford wasn't a purposeful decision, but rather a gradual evolution. Since 2014 they have offered a complete vaginal breech service. They have had 51 successful of 77 planned breech births.
They do 36 week growth scans at Oxford, which has allowed them to drastically reduce the number of undiagnosed breeches.
Where do you start in setting up a breech service?
- You’ve really got to know your stuff
- Give staff/colleagues exposure to breech training; seek out experts in the field
- Involve senior key obstetric and midwifery “influence-ors”
- Talk about it--generate interest
- Prepare guidelines, patient leaflets, care plans, and data collection forms
- Be prepared to learn
- Keep mom and baby at the center of decisions
- Be prepared to work as a multidisciplinary team
- Ensure 24/7 coverage to provide consistency in care
- Involve the pediatric team in preparation. Pediatricians have learned over the past several decades that breech birth is bad. We have to teach them again that breech is okay and that it can be done safely.
- Expect resistance & knockbacks
- Remain within labor guidelines. (Anita noted that these guidelines have been challenged recently. There are different opinions on which guidelines are absolutes and which may be open to revision.)
- Learn from your outcomes to improve the future (for example, a different pattern of labor can be okay).
Remember, it’s up to the women what to do.
Make sure the information given to women is consistent between providers so they aren’t getting mixed messages
Evidence on how to provide a safe service
They looked at the PREMODA study intensively, noting significant differences between the TBT and PREMODA protocols. Some of the main areas of difference were fetal monitoring, presence of an experienced attendant, prenatal ultrasound to look at head flexion and estimated fetal weight, pelvimetry, and length of labors. They strive to follow the same protocols as the PREMODA study.
How to do a breech the "right" way
The "right" mother has an engagement with active birth and goes into spontaneous labor at term.
The "right" baby is not too big and not too small, with a flexed or neutral head, and in extended or flexed breech presentation (i.e., not footling or kneeling).
The "right" way starts with the birth team who all follow these practices:
- no stretch & sweeps
- no augmentation
- minimal vaginal exams (ideally very few, sometimes none at all)
- careful auscultation
- awareness of critical birth signs (knowing the normal rotation & descent of the breech baby)
- observing for color, tone and perfusion of the baby as it is born – and intervening promptly if either any of these are cause for concern
- leaving the cord intact if at all possible. Anita explained that an intact cord helps a baby resuscitate itself. If you cut the cord on an asphyxiated baby, you interfere with the blood/brain circulation
Oxford's outcomes
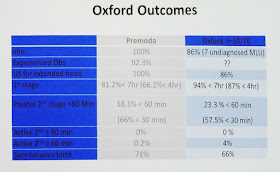
Anita ended by presenting Oxford's breech outcomes and comparing them against the PREMODA study.
57% of primips and 82% of multips planning a VBB had vaginal births. At Oxford the women tend to have quick 1st stages, with some passive 2nd stages.
The babies weighed between 2220g - 3860g. 94% had 5-minute Apgars >= 7. There were two cesarean-related complications (both postpartum hemorrhage) and 3 manual removals of the placenta. There were 2 episiotomies, 18 intact perineums, and no 3rd degree tears.

Their ECV clinic has a 50% success rate of turning breech babies head-down. Of the women with successful ECVs who went into labor with head-down babies, 70% of primips and 94% of multips had vaginal births.
~~~~~
Dr. Andrea Galimberti commented that these are very impressive figures. He's thinking back to the time before 2001 when vaginal breech delivery was the norm. He’s been talking with several people interested in setting up a breech service in their hospitals.



No comments:
Post a Comment